Laser Speckle Patterns and Malaria
Of the five different parasites that cause malaria, one type can cause death within hours of the observable symptoms.1 Current methods of detecting malaria take between 8 and 10 hours in the highest risk areas. A new technique, created by an international group, analyzes the speckle patterns of laser light reflected off of a blood sample with detection times of 30 minutes.2-3 Their innovation is likely to result in a fast, accurate, and portable device.
Figure 1.
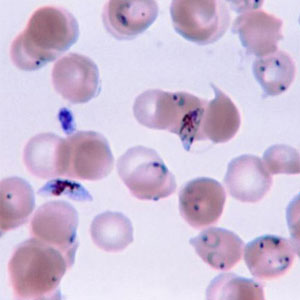 (a) Human blood with parasite causing malaria. Image credit: Wikimedia Commons |
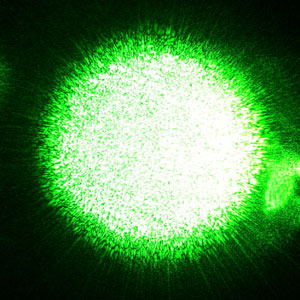 (b) Speckle pattern created by a laser. Image credit: Wikimedia Commons. |
What’s speckle?
Laser light is special. If you take a laser and point it at a small angle on a piece of paper, you’ll see that it creates a spot with very bright and dark parts. This is called a speckle pattern. An ordinary light source (which is usually spatially incoherent) does not do this. Laser light ideally has one wavelength and frequency (monochromatic), travels in the same direction (collimated), and all the light is in phase or in step (coherent). An analogy is a marching band, all in the same color uniform, perfectly lined up, headed in the same direction, and all marching in perfect step. Ordinary light sources consist of many different wavelengths (or colors), traveling in many directions, and they are not in phase (they are out of step). The special properties of laser light, along with how they interact with the surface they are striking, cause the speckle pattern. Most surfaces are not completely smooth. For example, paper is fibrous having hills and valleys. When light reaches the paper it reflects off of it, into our eye, and we perceive it. A light ray hitting one section of the paper (a valley) travels a different distance than a light ray hitting another portion of the paper (a hill). These two waves may be in step (in phase) or out of step (out of phase) when they reach our eye. If they are perfectly in step we see a very bright spot (constructive interference) and if they are perfectly out of step we see a black spot (destructive interference). For a regular light source there are so many different wavelengths, phases, and angles that the light strikes the paper and reflect off at, that by the time it reaches our eye (the detector) it averages out and the spot on the paper looks homogenous. For laser light, the differences in the distances the light rays travel before they reflect cause very distinct constructive and destructive interference patterns.4
How speckle is used to detect malaria
Using current methods specialists can image and detect the parasites within blood cells. However, the current method takes a lot of time and it is not portable. Time is critical in detection of malaria so the researchers are trying to create a fast, automated, and portable device. The international research teams led by Dan Cojoc5 (Italy), Zeev Zalevsky6 (Israel), and Vicente Mico7 (Spain), looked at healthy and infected red blood cells using traditional microscopic methods and a new system they are investigating. This new system analyzes the speckle pattern produced by shining a laser on the red blood cells. The system incorporates a microfluidic chip, a laser, a digital camera, and a computer to analyze the results.
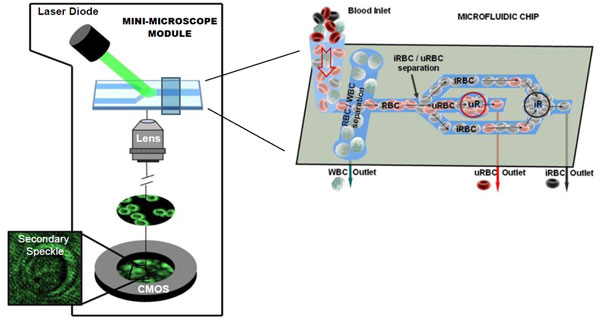
Figure 2.
A schematic of the device used by researchers. Notations: CMOS – Complementary Metal-Oxide Semiconductor camera (works like a ccd in that it converts incoming light into an electrical charge on a semiconductor), iRBC – infected Red Blood Cells, uRBC – uninfected Red Blood Cells, WBC = White Blood Cells. Image credit: The international research groups led by D. Cojoc, Z. Zalevsky, and V. Mico.
The researchers needed to determine the best distance at which to image the speckle pattern and which parameters of the cell structure would be the most significant to measure and analyze to determine if a cell is infected. The parasite responsible for malaria alters the host red blood cells during its life cycle, changing the structure and form of the cell. The cell becomes slightly stiffer and deformed.
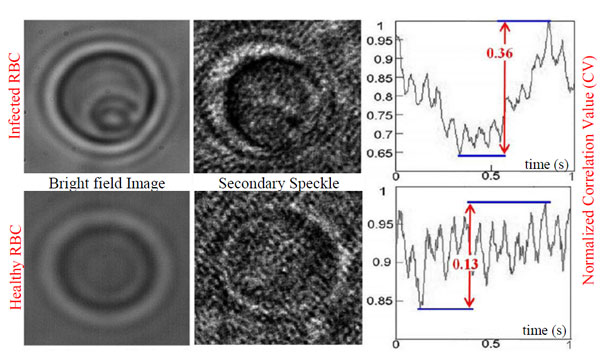
Figure 3.
The first row shows an infected red blood cell in which a trophozoite (one stage of the life cycle the parasite responsible for malaria) can be observed, and the second row shows a healthy red blood cell. Both bright field image and secondary speckle patterns are shown, along with the normalized correlation value. Image credit: The international research groups led by D. Cojoc, Z. Zalevsky, and V. Mico.
By considering a number of measurements on healthy and infected blood cells they found that the most likely determination of infected cells would show significant differences in at least one of a number of variables, but not necessarily each of the variables. All the variables that were inspected were related to correlation operations on the time varying speckle pattern. This set of variables was analyzed using two methods. The first method utilized fuzzy logic, which allows reasoning based on approximate rather than exact values to determine if a sample is infected. An automated system would need to check each of these variables and give back a result of "likely infected" or "likely healthy". They tested their program on their samples and found it to be close to 70% accurate in determining if cells were infected or healthy. The researchers considered a second analysis of the variables selected, utilizing a concept called Principal Component Analysis. This second method maps the variance of the correlated variables onto a new coordinate system. Using this method the researchers found a cutoff value, below which there was 100% accuracy in identifying healthy cells, and above the cutoff value there was above 85% accuracy in identifying infected cells (12 out of 14).
Current and Future Research
Analyzing speckle patterns began being utilized to determine real-time speed of blood flow for grafting surgeries in 2006.8 The use of speckle patterns described in this article is likely to lead to a portable, fast, precise, and accurate way to detect malaria. According to the World Health Organization’s 2011 report9 there were over 3.3 billion people at risk of malaria in 2010, and of the 216 million cases reported in 2010 about 655,000 people died from it. The main effort of the researchers will be directed into the development of a low cost, household malaria detection kit based on micro fluidic chips that provides automatic, sufficiently accurate results in a short time.
References and Links
1. A.D.A.M Medical Encyclopedia, Malaria, PubMed Health, U.S. National Library of Medicine, 9 June 2011
2. Cojoc, D., et. al, Toward fast malaria detection by secondary speckle sensing microscopy, Biomedical Optics Express 3(5), 991-1005 (2012)
3. Carts-Powell, Y., Spotting Malaria Fast, Optics & Photonics News, 23(78), 8, July/August 2012.
4. Doss, H, Lee. E, Plisch, M, The Physics of LASERs Inquiry Lessons for High School Physics Students, student and teacher editions, APS 2010.
5. Dan Cojoc’s research lab at Advanced Technology and Nanoscience National Laboratory (TASC), Trieste, Italy
6. Zeev Zalesky’s research lab at Bar-Ilan University, Ramat-Gan Israel
7. Vicente Mico’s research lab at Departamento de Optica, Universitat de Valéncia, Burjassot, Spain
8. Optics.org, Lasers light up blood-flow dynamics, 21 August 2006
9. World Malaria Report 2011 Fact Sheet, World Health Organization (WHO), December 2011
H.M. Doss